

The researchers concluded, “Processed electroencephalogram-guided general anesthesia management, consisting of PSi combined with DSA monitoring, can significantly reduce the risk of postoperative delirium in patients undergoing CEA. There was no significant difference in the incidence of other neurologic complications. Patients in the intervention group also spent significantly less overall time with EEG suppression. The researchers found that the incidence of POD was significantly lower in the intervention group (7.87% of patients) compared to the standard group (28.91% of patients, p < 0.01). A team of neurophysiologists independently reviewed the EEG data acquired by SedLine to calculate the cumulative duration of burst suppression for each patient. Secondary outcomes were postoperative hospital length of stay (LOS) and other neurologic complications. The primary outcome was the incidence of POD, measured using the Confusion Assessment Method, during the first three days after surgery.

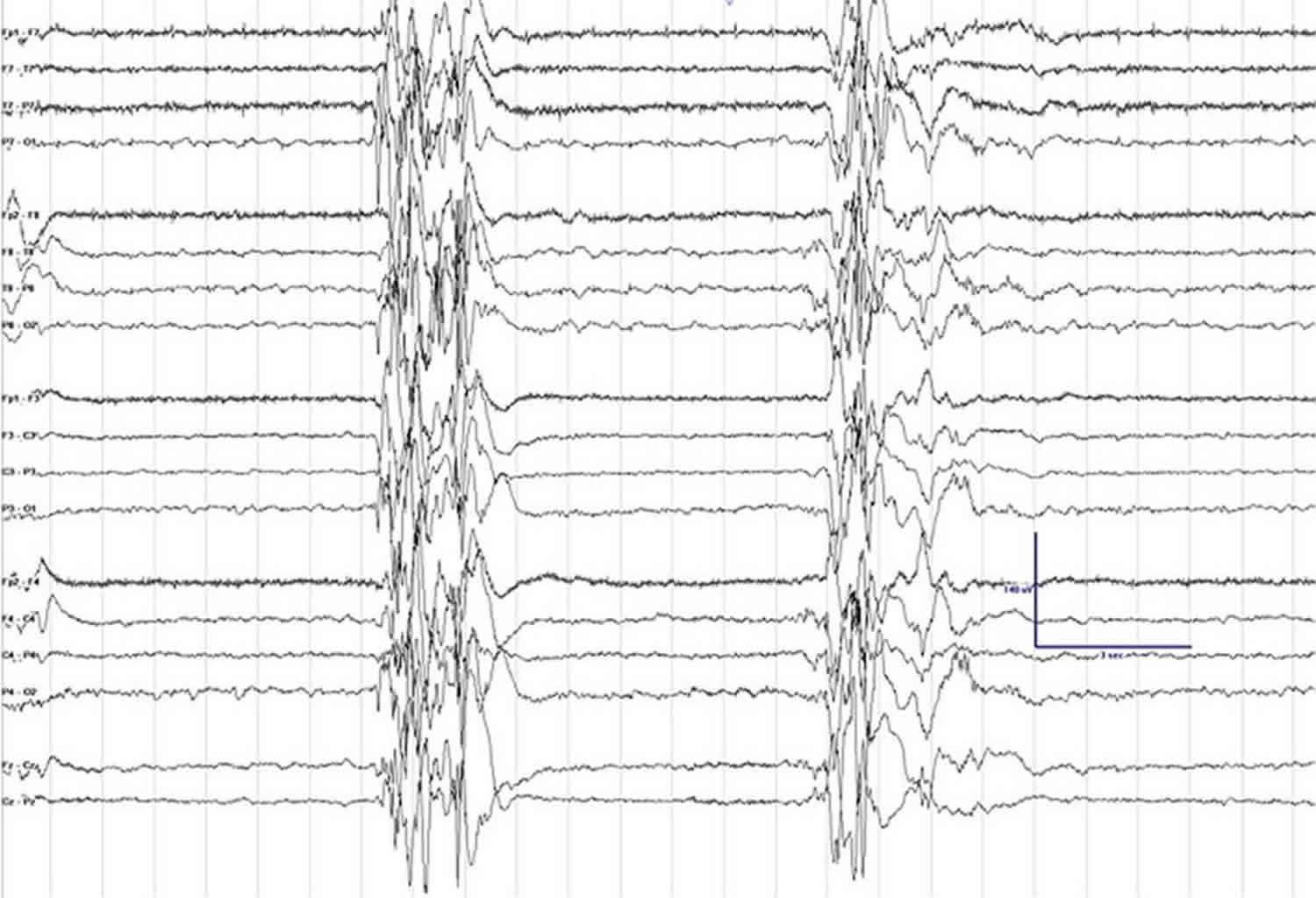
In both groups, patients were also monitored with continuous transcranial Doppler ultrasound and near-infrared spectroscopy (NIRS) (designed to avoid perioperative cerebral hypoperfusion or hyperperfusion). In the intervention group, general anesthesia was managed using a combination of Masimo SedLine PSi and DSA monitoring (designed to reduce the risk of intraoperative EEG burst suppression) in the standard group, PSi without DSA monitoring was used. The authors enrolled 255 patients scheduled for CEA and divided them randomly into an intervention group (n=127, mean age 62) and a standard group (n=128, mean age 63). Noting that the incidence of POD is associated with the duration of EEG suppression during surgery, they sought to investigate whether monitoring multiple processed EEG parameters simultaneously to guide anesthesia during a procedure like CEA could positively impact the incidence of POD, compared to use of a single parameter alone. POD is a “common yet serious” type of geriatric neurological dysfunction associated with worse short- and long-term prognosis and higher healthcare costs. The researchers noted that cerebral blood supply may be “severely disrupted” during CEA, the gold standard treatment for severe carotid stenosis, and that cerebral function is “highly vulnerable” to even brief changes in oxygen and blood supply, as well as to cerebral vascular diseases like carotid stenosis.


 0 kommentar(er)
0 kommentar(er)
